Clinical research is entering a new era. As trial complexity increases and medical evidence expands at an unprecedented pace, traditional research workflows struggle to keep up. AI clinical research tools are now reshaping how studies are designed, analyzed, and translated into real-world care—without compromising scientific rigor.
From protocol design to evidence synthesis, artificial intelligence is helping researchers work more efficiently while maintaining the standards required for high-quality clinical research. This article explores where AI fits into modern research workflows, its benefits, limitations, and why evidence-based AI matters more than ever.
What AI Clinical Research Means Today
AI clinical research refers to the use of artificial intelligence and machine learning to support—not replace—human-led research activities. In practice, this means applying AI to help researchers and clinicians work through growing volumes of data while maintaining scientific rigor and transparency.
Modern AI clinical research tools are commonly used to:
- Identify and prioritize relevant clinical studies and datasets
- Analyze large, complex research outputs more efficiently
- Support protocol development and endpoint selection
- Synthesize evidence from trials and real-world data
- Translate research findings into clinically meaningful insights
Crucially, clinically responsible AI systems are grounded in verified medical literature, traceable reasoning, and research-aware design. This distinction is explored in more depth in ZoeMD’s article on medical research AI, which outlines how AI can accelerate research workflows without compromising evidence quality.
How evidence-based AI reduces hallucinations: Retrieval-Augmented Generation (RAG)
Many evidence-based clinical research tools use a Retrieval-Augmented Generation (RAG) approach to keep outputs reliable. Rather than relying only on a model’s “memory,” the system first retrieves relevant passages from vetted medical sources, then generates an answer grounded in that retrieved evidence. This reduces hallucinations by anchoring responses to what was actually found and enables transparent citations back to the underlying material.
In this context, AI functions as a research accelerator—helping teams manage complexity, surface relevant evidence faster, and focus more time on interpretation, validation, and scientific decision-making.
Why AI Matters in Modern Clinical Research
The volume of medical research continues to grow exponentially. Thousands of trials, observational studies, and systematic reviews are published every year, making manual synthesis increasingly impractical.
AI clinical research tools help address several core challenges:
1. Research overload
AI can scan and organize vast bodies of literature far faster than manual review, surfacing relevant studies while filtering out low-quality or outdated sources.
2. Trial complexity
Modern studies often involve multimorbidity, stratified populations, and adaptive designs. AI systems can help researchers explore complex variable relationships without oversimplifying results.
3. Time-to-evidence pressure
Regulators, clinicians, and patients all expect faster insights. AI-assisted analysis shortens the gap between data collection and actionable findings.

Key Applications of AI in Clinical Research
Study design and protocol development
AI tools can analyze prior trials, endpoints, and inclusion criteria to help researchers design more efficient and statistically sound protocols. By identifying what has—and hasn’t—worked before, AI reduces trial redundancy and improves feasibility.
Evidence synthesis and literature review
One of the most practical uses of AI clinical research is rapid evidence synthesis. AI can summarize clinical trials, meta-analyses, and guideline updates while preserving citation integrity. This mirrors the same evidence-first philosophy used in ZoeMD’s clinical decision support workflows.
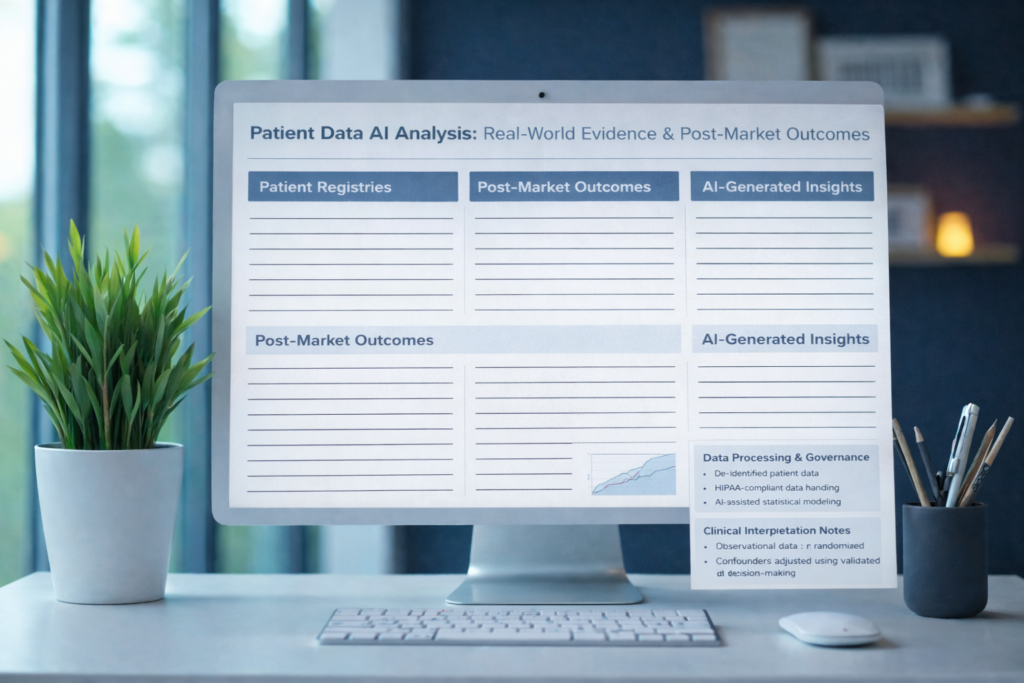
Real-world evidence analysis
Beyond traditional trials, AI can help analyze real-world data such as registries, EHR-derived datasets, and post-market surveillance information—supporting a more complete understanding of treatment outcomes.
Translational research support
AI bridges the gap between research and practice by helping researchers contextualize findings within current guidelines and clinical standards, a key requirement for real-world impact.
The Importance of Evidence-Based AI in Research
Not all AI tools are appropriate for clinical research. General-purpose models may generate plausible-sounding outputs that lack scientific grounding, reproducibility, or traceability.
Why RAG improves trust and auditability
RAG adds an explicit “evidence retrieval” step before answer generation. In practice, a query triggers a search across a controlled knowledge base (e.g., guideline repositories, curated literature collections, or approved internal documents). The system then selects the most relevant excerpts, and the model composes the response using those excerpts as its reference frame.
For clinical research workflows, this matters because it:
- Limits unsupported claims: if the retrieval step doesn’t surface strong evidence, the system can narrow the answer, express uncertainty, or recommend reviewing primary sources.
- Improves traceability: citations can be tied to specific passages, enabling faster verification and internal review.
- Supports reproducibility: the retrieved evidence can be logged (with versioning) so teams can understand what the system used at the time of answering.
Evidence-based AI platforms prioritize:
- Verified medical sources
- Transparent reasoning pathways
- Alignment with established clinical guidelines
- Clear distinction between evidence and interpretation
ZoeMD’s platform reflects this approach by focusing on research-backed reasoning rather than opaque predictions. Researchers and clinicians can explore how this model works in practice through the Evidence-Based Medical AI overview.
Regulatory and Ethical Considerations
AI clinical research must operate within strict ethical and regulatory frameworks. Key considerations include:
- Data privacy and security
- Bias detection and mitigation
- Reproducibility of results
- Clear human oversight
AI should support regulatory compliance—not complicate it. Systems designed with healthcare regulations in mind are far more likely to gain institutional trust and long-term adoption.

How Clinical Researchers Can Start Using AI Responsibly
A practical approach to AI adoption in research includes:
- Start with a narrow use case
For example, accelerating literature reviews or evidence synthesis. - Validate outputs against known evidence
AI insights should always be cross-checked with primary sources. - Maintain human decision authority
AI supports judgment; it does not replace peer review or scientific accountability. - Choose evidence-first platforms
Tools built for healthcare research outperform generic AI systems in reliability and trust.
Researchers interested in exploring AI tools that align with clinical standards can also review ZoeMD’s pricing options or reach out directly via the contact page for platform details.
Final Thoughts
AI in clinical research is no longer about experimentation or hype—it’s about precision, efficiency, and trust. As studies become more complex and evidence continues to grow at scale, researchers and clinicians need tools that can keep pace without sacrificing scientific rigor.
When grounded in verified sources and transparent reasoning, AI clinical research tools help teams move faster from data to insight, reduce manual workload, and ensure findings remain aligned with current guidelines and real-world clinical standards. The key is choosing AI platforms that are built specifically for healthcare—not generic systems retrofitted for medicine.
ZoeMD is designed with this exact principle in mind: supporting research and clinical workflows through evidence-based AI, clear sourcing, and clinician-first design.
If you’re exploring how AI can responsibly support clinical research and evidence interpretation, here are a few ways to get started:
- Learn how ZoeMD approaches research-grade AI on the Evidence-Based Medical AI page
- Review pricing options for individuals, teams, and organizations involved in research or clinical programs
- Reach out via the contact page to discuss research use cases or request a walkthrough
- Find answers to common questions about data sources, methodology, and compliance in the FAQs
As clinical research continues to evolve, the most effective teams will be those that combine human expertise with evidence-first AI tools. ZoeMD helps ensure that AI enhances research quality—without compromising accuracy, accountability, or clinical judgment.


